Let’s dive into vital signs. When you think of vital signs, most people think of blood pressure, respiratory rate, and pulse. But there’s so much more to it. Let’s break it down with detailed explanations and examples.
Part 1: Responsiveness Assessment
We assess responsiveness using the AVPU scale and Glasgow Coma Scale (GCS).
AVPU Scale
- Alert: The patient is awake and responsive. For example, they can answer questions coherently.
- Verbal: The patient responds to verbal stimuli, like when you call their name or give a command.
- Pain: The patient only responds to painful stimuli, such as a pinch or pressure applied to the nail bed.
- Unresponsive: The patient does not respond to any stimuli, indicating a deeper level of unconsciousness.
Glasgow Coma Scale (GCS)
The GCS ranges from 15 (fully alert) to 3 (deeply unconscious). It assesses:
- Eye Opening (E): Scored from 1 to 4 (spontaneous opening gets 4 points).
- Verbal Response (V): Scored from 1 to 5 (oriented conversation gets 5 points).
- Motor Response (M): Scored from 1 to 6 (obeying commands gets 6 points).
Example: A patient with spontaneous eye opening (4), confused conversation (4), and obeying commands (6) would score 14 on the GCS.
Part 2: Respiratory Assessment
Assessing respiration involves more than just counting breaths per minute. We must also evaluate the quality, depth, and use of tools like pulse oximetry and end-tidal CO2 (EtCO2) monitors.
Respiratory Rates
- Adults: 12-20 breaths per minute
- Adolescents: 12-16 breaths per minute
- School-aged Children: 18-30 breaths per minute
- Preschoolers: 22-34 breaths per minute
- Toddlers: 24-40 breaths per minute
- Infants: 30-60 breaths per minute
Pulse Oximetry (SpO2)
Measures oxygen saturation in the blood. A normal range is 94–99%. Be cautious in cases like carbon monoxide poisoning, where SpO2 might be misleading because CO binds to hemoglobin more effectively than oxygen.
End-Tidal CO2 (EtCO2)
Essential for confirming intubation and monitoring respiratory status. A normal range is 35–45 mmHg. It’s crucial in assessing patients with altered mental status or respiratory issues.
Part 3: Cardiovascular Assessment
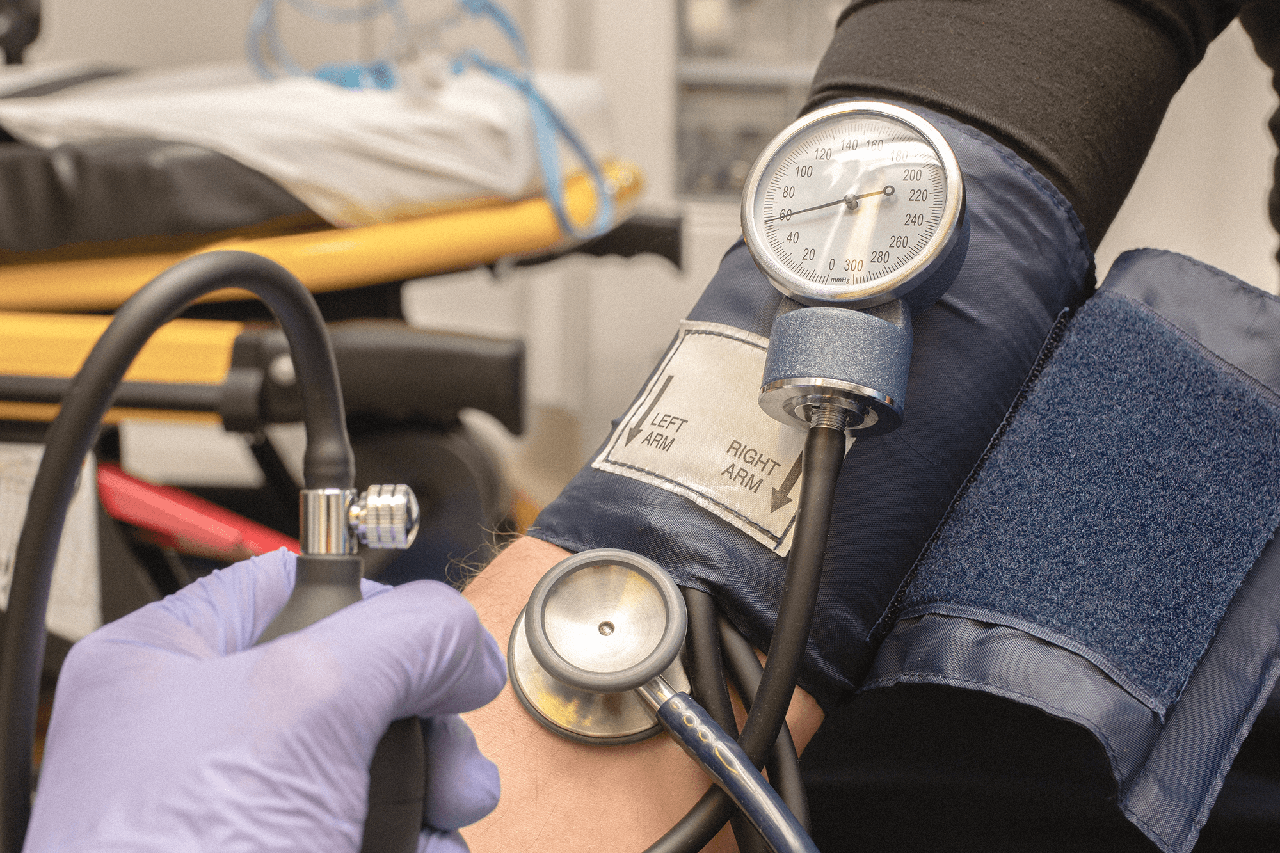
Blood Pressure
Blood pressure gives us the systolic (top number) and diastolic (bottom number) pressures.
- Normal Adult Blood Pressure: Around 120/80 mmHg is considered normal.
- Normal Pediatric Blood Pressure:
- 1-28 days: systolic BP of at least 60 mmHg
- 1 month to 1 year: systolic BP of at least 70 mmHg
- 1 year to 10 years: 70 + (2) age (For example, an 8-year-old should have a systolic BP of at least 86 mmHg.)
- 10+ years: systolic BP of at least 90 mmHg
Pulse and Heart Rate
Pulse and heart rate are closely related but not the same. Pulse is what you feel, while heart rate is what you monitor.
Normal Heart Rates by Age
- Adults: 60–100 beats per minute
- Children: 60–140 beats per minute (varies with age)
- Infants: 85–205 beats per minute
Part 4: Other Assessments
Pupil Assessment
Pupil assessment uses the PEARL acronym: Pupils Equal And Reactive to Light.
- Constricted Pupils: Can indicate opiate overdose.
- Dilated Pupils: May suggest stimulant use or other conditions like brain injury or shock.
Blood Glucose Levels
Blood glucose levels are vital, especially in patients with altered mental status or diabetes.
- Normal Levels: Range from 80–120 mg/dL.
- Hypoglycemic: Symptoms of hypoglycemia typically appear below 60 mg/dL. Watch for signs like confusion, sweating, and tremors.
Neurogenic Functions
A quick neuro exam includes checking all four extremities’ pulse, motor, and sensory functions.
- Pulse: Feel for pulses in all extremities to ensure proper circulation.
- Motor Function: Assess grip strength and foot movement.
- Sensory Response: Check for the ability to feel touch in various body parts.
- Neurological Function: Ask questions related to person, place, time, and event. For example, what is your name, where are you at? What day of the week is it? Can you tell me what happened?
And that’s our extended review of vital signs. Each of these components gives us a fuller picture of our patient’s health. Let’s make sure we’re thorough in our assessments to provide the best care possible.

